EffectivePhysio
Sue Cowley - Physiotherapy & Acupuncture
Welcome to EffectivePhysio
EffectivePhysio is a physiotherapy service in the Horsham area run by Sue Cowley, an experienced physiotherapist in musculoskeletal physiotherapy and acupuncture. Sue owned a successful physiotherapy clinic in Hertfordshire for 6 years before moving to Horsham in July 2014.
At EffectivePhysio treatment is based on a thorough assessment and the patient‘s own goals. The aim is to regain function and prevent further reoccurance.
People of all ages and backgrounds with muscle, joint and/or soft tissue problems are treated at EffectivePhysio.
No referral necessary.
Home visits available.
Read our Latest News & Updates

Have you been experiencing persistent aches, pains, or mobility issues? It might be time to consider seeking help from a physiotherapist. Here are five signs that indicate you may benefit from the expertise of a physiotherapist: 1. Nagging Aches and Pains If you've been dealing with persistent aches and pains that don't seem to improve after a week or two, it's a clear sign that seeking guidance from a physiotherapist could be beneficial. While it's normal to experience soreness after intense physical activities, ongoing and unrelenting pain may require professional attention. 2. Pain at Your Desk Sitting at a desk for extended periods can lead to discomfort, such as backaches or headaches. If you find yourself experiencing pain while at your desk, it's essential to address these issues to prevent further strain on your muscles and joints. Regular breaks and proper desk ergonomics can help, but if the pain persists, consulting a physiotherapist is advisable. 3. Constant Pain Experiencing constant pain, whether it's related to a specific movement or a general discomfort, is a significant indicator that you may need physiotherapy. Ignoring persistent pain can lead to further complications, making it crucial to seek professional assessment and treatment. 4. Delayed Recovery If you've sustained an injury and notice that the pain persists beyond the expected recovery period, it's a clear indication that professional intervention may be necessary. Physiotherapists can assess the underlying issues and provide targeted exercises and rehabilitation programs to facilitate recovery. 5. Limited Mobility Struggling with limited mobility, whether due to an injury, chronic condition, or other factors, can significantly impact your quality of life. Physiotherapists can develop tailored treatment plans to improve mobility, reduce pain, and enhance overall function, helping you regain your independence and well-being. Recognising these signs and seeking timely assistance from a physiotherapist can play a crucial role in managing and addressing physical discomfort and limitations. Remember, it's essential to prioritise your well-being and seek professional guidance when needed. If you resonate with any of these signs, it may be time to consider scheduling a consultation with a qualified physiotherapist to address your specific needs and embark on a path towards improved physical health and well-being.

Training for Running Events: Top Tips from EffectivePhysio As we approach April, many runners are in the midst of their training schedules for upcoming marathons. Whether you’re a seasoned runner or a weekend warrior, preparing for a running event can be a daunting task. Here at EffectivePhysio, we’ve compiled some top tips to help you train effectively and safely. 1. It’s an Event, Not a Race Firstly, it’s important to remember that these are running events, not races. Races are for professionals or running enthusiasts aiming to improve their personal bests. Our advice is geared towards those who want to participate in occasional events like half marathons, 10Ks, or even, marathons. 2. Follow a Plan There are numerous training plans available, most of which include a long run once a week, a speed/interval training run once a week, and a shorter, jog run once a week. The speed training involves running at 80% of your maximum effort for an increasing period, followed by a reducing walking period. 3. Prevent Injuries In our experience, injuries are more likely to occur during speed training. Ensure you walk for enough time after your sprint to allow your muscles to recover, even if you’ve recovered aerobically and caught your breath. 4. Start Early Start your training early so you can pace yourself and gradually increase your mileage. If you’re training for the April marathons, you should aim to run 10 miles by the beginning of January. Building up an extra mile each week on your long run is a good strategy. 5. Strengthen Your Muscles Perform strengthening exercises twice a week for your legs and arms to protect against injury. Key running muscles include the glutes (both maximus and medius), quads, and calf muscles (especially the soleus). Recommended exercises include squats, bridging, leg press, dead lifts, and heel raises. 6. Warm Up Before your run, do a few squats to engage the glutes, quads, and hamstrings, and a few heel raises to engage the calf muscles. 7. Stretch Stretching after a run is crucial. Target both calf muscles (gastroc and soleus), quads, hamstrings, adductors (groin muscles), and piriformis (a muscle deep in your buttock). 8. Check Your Body During your long runs, perform a body check every 3-4 miles to ensure your joints and muscles are comfortable. Check your posture and make sure you’re not leaning forward, bracing your upper back, or tensing your shoulder muscles. 9. Rest Feeling muscle ache as the weeks progress is normal. Rest is as important as the runs, so build a ‘rest’ week into your training schedule to let your muscles recover. 10. Don’t Worry About Arthritis If you have arthritis in your joints, don’t worry. Research has shown that moderate running with moderate arthritis is okay, as long as you pace yourself and gradually build up the miles. 11. Deal with Injuries If you feel you’ve injured your muscles, usually going easy for 1-2 weeks with 5k jogs and reduced weight strengthening should ease this. Try taking shorter running steps to take the stress off the leg muscles. Stretching and applying ice packs to the sore muscles can also help. If an injury lasts longer or isn’t recovering as fast as you’d like, it may be beneficial to see a physiotherapist. Please phone EffectivePhysio on 07719987520! Remember, the key to successful training is consistency, patience, and listening to your body. Happy running!
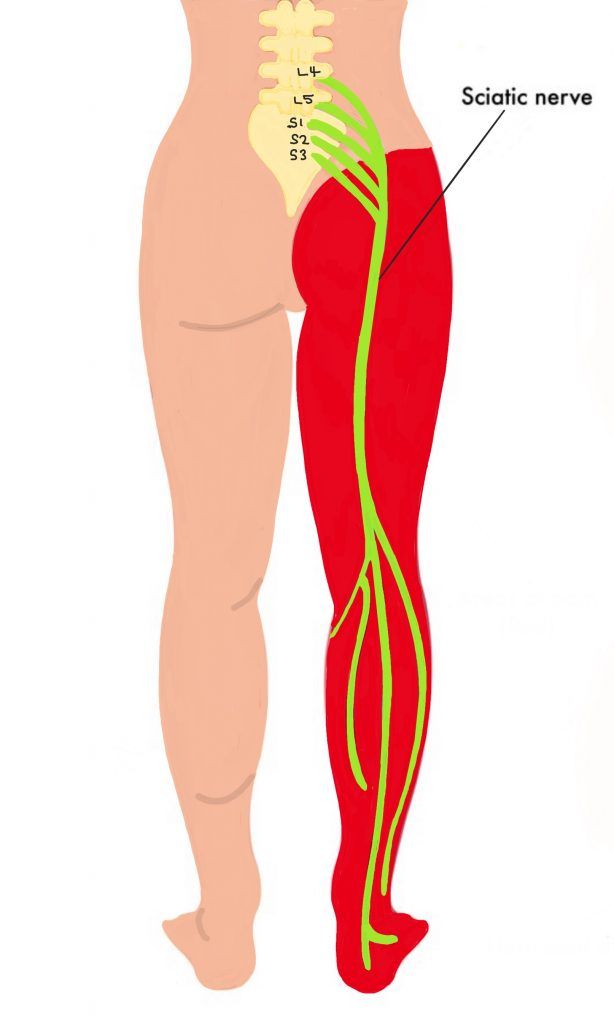
What Is Sciatica? Sciatica is the symptom of pain radiating from the lower back or buttock area to the posterior or outer side of the leg down to the feet and even the big toe. The sciatic nerve becomes irritated or compressed at some point along its course. Common Symptoms include: Pain in the buttocks, back of the leg, foot, and toes. The distance the pain travels down the leg is an indication of the severity of the compression or irritation of the nerve. The pain may feel like stabbing, burning, or shooting. Tingling sensations (like pins and needles) or numbness. Weakness in the affected leg. Pain worsens with movements in certain directions. Other movements may ease the pain. Back pain may or may not accompany sciatica. Causes of Sciatica: Bulging Discs (Herniated Disc): A bulging or herniated disc compresses the sciatic nerve. Inflammation / scar tissue of soft tissues such as ligaments around facet joints (the wing joints either side of the disc joint at each level of your spine) or the pelvic joint may ‘tether’ the nerve and prevent it gliding through the tissues smoothly causing the nerve (the structure telling your brain there is pain) to be irritated. Piriformis Syndrome: Tightness or spasm of the piriformis muscle deep in the buttock area. Lumbar Spinal Stenosis: Narrowing of the spinal canal, putting pressure on the nerve. Spondylolisthesis: Vertebrae slipping out of alignment. Pregnancy: Pressure on the sciatic nerve due to changes in the body during pregnancy. How Can Physiotherapy Help? The physiotherapist will assess you to find out what is compressing or irritating the sciatic nerve and tailor treatment according to the findings. Exercise Prescription: A physiotherapist will design a personalized exercise program. Strengthening exercises for core muscles to control any movements that are ‘giving’ and therefore putting strain on the tissues. Stretching exercises to improve flexibility, minimise stiffness and reduce nerve compression / tethering. These exercises are often the ones that give ‘first aid’ pain relief. Exercises to glide the nerves to reduce tethering and therefore pain. Manual Therapy: Techniques like joint mobilization and soft tissue techniques to help the sciatic nerve move freely within its structures. Acupuncture may also be used. Posture Correction: Proper posture during sitting, standing, and lifting. Avoiding prolonged sitting. Self-Care Tips: Heat Packs: Apply heat to your lower back. Cushioning: Use a small, firm cushion between your knees while sleeping on your side. Gentle Exercise: Start moving as soon as possible, for example, with short, gentle walks gradually increasing the distance. Pharmaceutical Support: Consult a pharmacist for suitable painkillers. When to Seek Medical Attention: Severe pain or worsening symptoms. Weakness or numbness in both legs. Numbness around genitals or difficulty urinating. Loss of bowel or bladder control. Remember, early intervention and appropriate management can significantly improve sciatica. If you experience sciatica, consult a physiotherapist if symptoms do not improve with home treatments within 1 to 2 weeks. Physiotherapy for back pain and sciatica is available privately at EffectivePhysio. Call 07719987520.